There are some. glaucomaVision loss in patients continues despite treatment. New research from China indicates that immune cells are migrating from the digestive tract into the eyes.
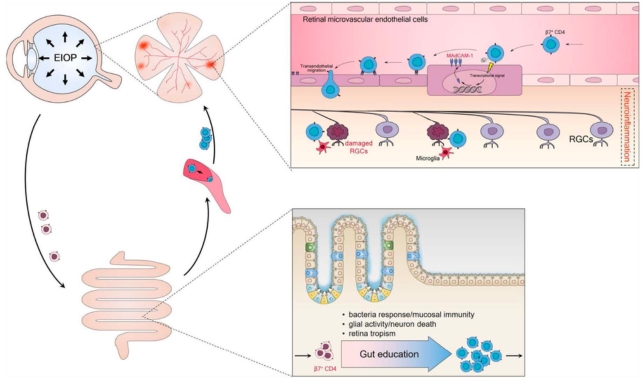
These “gut retina axis” (or “gut-retina”) cells bind specific proteins and gain access to eye’s Light-sensitive tissuesThey damage retinal ganglion cells (RGCs).
Glaucoma, The group of diseases known as neurodegenerative diseaseIt is a term used to describe eye conditions caused by loss RGCs. RGCs are the cells that form the retina. A nerve that is visibleThis transmits visual data to the brain.
The optic nerve sends this information to the brain visual cortexYou can process this right now if you read with your eyes.
You can also find out more about the A-Team here. Leading cause of blindnessGlaucoma, as it is known today, is incurable. Treatment aims to stop the disease progressing.
The researchers said that “our findings highlight the importance of gut-retina in glaucoma and the development of therapeutic approaches.” WriterThey have a paper.
Eye pressure is also known as Increased intraocular Pressure(EIOP), the main risk for glaucoma. Treatment aims to reduce EIOP, but this doesn’t stop progression of the condition.
Previous studiesImmune system is a hint T-cellsYou can learn more about it here Take a partIt is not known how glaucoma damages are caused.
Normal permission is normally refused to T cells and other immune cells circulating in the retina. NotesThe research team was led by the clinical immunologists Chong Xiu Wenbo Chen Qinyuan Chen and Kun Peng of the University of Electronic Science and Technology.
Four scientists from a group of four were involved in a Study of 2021This subset was found to be CD4+T cells“Express a” gut-homing receptor, integrin β7The protein, called, helped the virus to enter the retina. The mucosal molecule that is responsible for cell adhesion. (MAdCAM-1).
In their new study, He, Xiu, and team confirmed a link between CD4+ T cells that express integrin β7, MAdCAM-1, and glaucoma disease severity in patients.
First, blood samples were taken from 519 patients with glaucoma and 189 healthy control subjects. A significantly higher percentage of β7-expressing CD4+ T cells was found in glaucoma patients compared to healthy controls, and glaucoma patients with more of these cells in their blood had more severe eye damage.
Using an EIOP-induced mouse model of glaucoma, researchers next showed that to gain access to the retina, β7+ CD4+ T cells in these early stage glaucoma mice must make a detour through the gut.
The team found the β7+ CD4+ T cells of EIOP-induced mice were reprogrammed in the gut, so they could use integrin β7 as a kind of license, returning to the blood circulation functionally equipped to travel to the retina.
The gut-licensed T cells, however, were able bind MAdCAM-1, giving them access to eye tissue.Neuroinflammation can eventually lead to a neuroinflammatory condition“.
“The ability of MAdCAM-1 to induce expression on retinal [vessels] might be one of the mechanisms whereby gut-licensed β7+ CD4+ T cells cross the blood-retina barrier and invade the retina,” the team Explained.
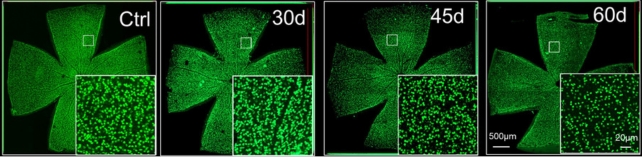
The team administered a glaucoma test to investigate the relationship between these cells and proteins. antibodies to mice that blocked the β7+ CD4+ T cells’ interaction with MAdCAM-1. Glaucoma damage was reduced by blocking the MAdCAM-1 interaction.
“Our study reveals a role of gut-licensed β7+ CD4+ T cells and MAdCAM-1 in retinal ganglion cell degeneration,” the authors Writer.
It’s unclear how EIOP increases levels of these β7+ CD4+ T cells in the blood and how they are reprogrammed in the gut, so more research is needed.
The team concluded that clinical trials could be conducted to test whether antibodies used in the study could treat glaucoma. They also said their work demonstrates the possible role of the immune systems in diseases such as glaucoma.
The study was published by Science Translational Medicine.


